For an oversexed culture that isn’t afraid to push boundaries on TV, in movies, on the radio, and in books and magazines, we’re awfully shy about sex when it comes to our health. In fact, even though people with diabetes are at a higher risk for sexual problems, a 2010 study in the journal Diabetes Care found that only about half of all men with diabetes and 19 percent of women with diabetes have broached the topic with a doctor.
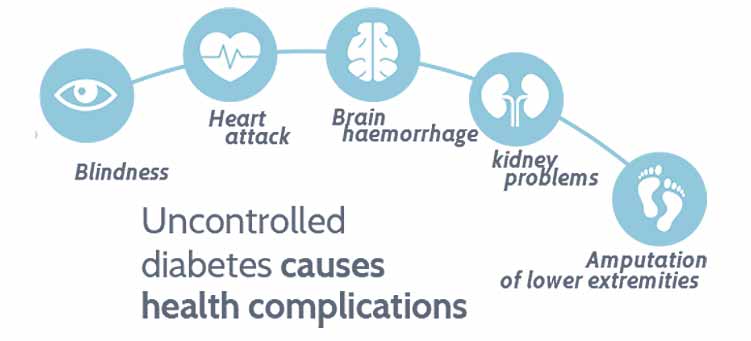
And, truth is, many doctors don’t feel comfortable prodding patients for details on sexual function. It’s why the newly diagnosed quickly learn about eye, nerve, kidney, and heart damage from uncontrolled diabetes, but hardly ever hear how diabetes affects sexual health. It is important for people to be open and honest with their doctors regarding all health concerns—even problems with sexual function. Problems with sexual performance and satisfaction can signal other health issues.
Many men with erectile dysfunction, for instance, later learn that they have diabetes. For people who already have diabetes, sexual problems can indicate nerve damage, blocked arteries, and even out-of-whack hormones. Though there’s a lot yet to learn about sexual dysfunction in people with diabetes, researchers are certain of one thing: Chronic high blood glucose is behind many sexual problems people face, and the first line of action is to improve glucose control.
Honey, Not Tonight
Low libido, or sexual desire, is a real problem, one that affects people with diabetes more than those without. Men and women experience low libido as a result of poorly controlled diabetes. If your sex drive is stalled, first look to your diabetes control and take steps to lower your blood glucose levels. Then consider your medications. Certain drugs, such as antidepressants, can lower sexual desire, so talk to your doctor.
Researchers theorize that inflammation may also dampen desire. “Sexual desire is a brain-driven event,” says Stacy Tessler Lindau, MD, MAPP, director of the Program in Integrative Sexual Medicine at the University of Chicago. “If inflammatory molecules cross the blood-brain barrier and circulate in the area where there is sexual desire, then it’s plausible the desire for sex may be affected.” Another possible culprit: low testosterone, which often affects men and women with diabetes.
Him:
Studies have shown that men with diabetes, especially those who have type 2 or are overweight, or both, have about twice the risk of low testosterone as their peers without the disease, which can affect a man’s passion for sex. “The treatment is to give testosterone, and it’s amazing how that can work in diabetes,” says Irwin Goldstein, MD, director of San Diego Sexual Medicine at Alvarado Hospital and editor in chief of The Journal of Sexual Medicine. When low testosterone is treated through losing weight and/or testosterone therapy, many men have a renewed desire for sex.
Her:
Treating women isn’t quite as simple. (Get used to hearing that.) Some studies suggest that taking testosterone can increase sexual desire in women—a 2008 article in the New England Journal of Medicine found that post-menopausal women had a greater sexual appetite after taking testosterone for almost six months—but the treatment is still understudied, particularly its long-term effects on women’s health. Not only that, but it’s hard for researchers to determine whether a particular woman’s low libido is a result of diabetes, emotional issues, or something else because low libido is common in women regardless of the presence of diabetes.
Let’s Get It On—Or Not
Here’s the difference between desire and arousal: First, sexual desire must occur; the body then responds, signaling arousal. That is, if everything’s working properly. Both men and women with diabetes may feel desire but struggle with arousal problems, though the mechanisms behind this sexual dysfunction are better studied and understood in men. For both men and women, a good place to start looking for possible causes is your medicine cabinet. Some blood pressure–lowering medications, for instance, can contribute to erectile dysfunction. When meds aren’t behind a person’s hampered arousal, diabetes may be to blame. Poor diabetes control over time can damage the blood vessels and nerves—as it does in heart disease and neuropathy (nerve damage), other complications of the disease—that make arousal possible.
Him:
One of the main sexual problems men with diabetes face is the inability to have an erection. Damage to the vascular system can impair blood flow. If the blood vessels aren’t functioning properly or if an artery is blocked, not enough blood will travel to the penis, making it difficult to get an erection.
Nerve function plays a role, too. If the brain isn’t properly communicating with the nerves in the sexual organs, the body might not be able to shuttle blood there, impairing a man’s ability to get an erection. The ability to keep an erection can also be affected, because the brain must communicate with the nerves to hold blood in the penis. (Keep in mind: A man’s ability to get and hold an erection typically wanes with age.)
Fortunately, there are plenty of treatment options. Neither men nor their partners should accept male sexual dysfunction, says Janis Roszler, RD, CDE, LDN, a certified diabetes educator and author of the book Sex and Diabetes: For Him and for Her. “For men, there absolutely is a treatment that will work.” Options include PDE5 inhibitors, such as Viagra and Cialis, which improve blood flow; testosterone injections or gels (if testosterone levels are low); injectable medications or suppositories; constriction rings that sit at the base of the penis; vacuum pumps that draw blood into the penis; support sleeves that hold the penis in place during sex; and penile implants.
Her:
Nerve damage may also cause vaginal dryness, which is twice as common in women with diabetes as it is in women without diabetes. It’s also a result of aging. “Vaginal dryness is very common among women who are menopausal or post-menopausal,” says Lindau. In those cases, a lack of estrogen is behind the dryness, and problems may be treated with prescription estrogen, available in pills, a patch, or a cream used in the vagina.
Because researchers don’t understand exactly why women’s bodies lose the ability to self-lubricate when menopause isn’t the cause, treatment options are slim. Most experts recommend using store-bought lubricant.
Women with diabetes are also prone to the same blood-flow issues men face because of nerve or blood vessel damage. Diabetes complications may make it difficult for blood to move to the vagina and clitoris. “The question we have, as far as women go, is that there are women with excellent A1Cs who don’t have any blood vessel issues,” says Roszler. “They don’t have any neuropathy. But they still have sexual problems.”
Because studying female arousal problems is difficult for many reasons—women may have a hard time determining just how turned on they are, and there’s less of a physical sign of arousal in women than there is in men—treatments are few. But Goldstein says research is promising.
A small study in the August issue of The Journal of Sexual Medicine found that women with type 1 diabetes who took 5 mg of tadalafil (Cialis) for 12 weeks reported an improved quality of life, greater arousal and orgasm, more enjoyment and satisfaction from sex, and more frequent sex. This doesn’t mean you should start sneaking your partner’s pills—please don’t: The treatment is unapproved in women, dangerous in some people with heart problems, and generally unsafe until proved otherwise. But it does show promise for female treatments of the future. As for the present, Lindau says some women use clitoral pumps to aid blood flow but notes that the device isn’t for everyone.
The Big O
An orgasm is a sought-after sexual reward, but for people with diabetes it can feel like an unattainable goal. And, yes, we’re talking about women and men here. Both can struggle with the elusive O, and the first thing they and their doctors should check are the medications they take, such as antidepressants.
Her:
Though women in general report more difficulty having an orgasm than men, those with diabetes have even greater difficulty. Sure, a woman’s inability to climax often has to do with her mental or emotional state (more on that later), but diabetes may be in play, too. According to a study published this August in the journal Obstetrics & Gynecology, middle-aged women whose diabetes requires insulin are 80 percent more likely to report trouble reaching an orgasm than women without diabetes.
“To the best of what we know now, the neurovascular system is necessary for arousal and orgasm,” says Lindau. “If the small nerves are not working properly, then you can have sensation problems. In order for the clitoris to have the engorgement it needs to orgasm, it needs to have the blood flow and sensation.”
A hormone imbalance may be to blame, Roszler says. Some scientists studying women’s ovulation cycles hypothesize that off-balance hormones, and not just testosterone, may be behind women’s decreased arousal and orgasm, but the research is in its infancy.
Him:
Having an orgasm is usually pretty easy for men, which is why it can be so frustrating if a man’s unable to finish. Like women, men suffering from neurovascular damage—and the lack of blood flow and/or sensation it creates—can have a hard time reaching an orgasm. Men can get around erectile dysfunction with a variety of treatments, ranging from medications to vacuum pumps, but these treatments will not fix neuropathy.
Putting On The Brakes
Sex is supposed to bring you and your partner pleasure, so pain is an indication that something isn’t right. Even if you’re shy, it’s important to discuss issues of painful sex with a doctor. “See a doctor who is familiar with taking care of sexual problems because we can rectify problems in [most] patients, especially people with diabetes,” Goldstein says.
Him:
Men with diabetes are at an increased risk for developing Peyronie’s disease, a condition in which scar tissue inside the penis causes a curved and painful erection. Before you worry, take heart: Penises all vary in shape, and a little curve isn’t a big deal. With Peyronie’s disease, the curve or bend is significant and can make having sex and getting or keeping an erection difficult and painful. A doctor can advise whether you should wait it out, take medication, or have surgery.
Her:
Having sex with too little lubrication can make a woman scream—and not in a good way. Vaginal dryness is one of the main reasons women with diabetes have pain during sex, and better lubrication is the answer. Whether that comes in the form of estrogen therapy for women whose dryness is a side effect of menopause or over-the-counter lubricants, the goal is to be well lubricated before sex.
Women with diabetes are also at a greater risk for urinary tract infections (UTIs) and vaginal yeast infections, which in turn may lead to painful sex. (Rest assured, though, that people with diabetes are at no greater risk of sexually transmitted diseases than those without the disease.) Lower your chances of getting a UTI or yeast infection by keeping your blood glucose under good control, and head to the doctor at the first sign of discomfort.
Sexual Healing
So maybe your sex life isn’t where it should be. If you can admit that to your health care provider, you’ve already fought half of the battle. Depending on the extent of your sexual dysfunction, you may be able to see improvement by getting your blood glucose in control. Even if the complications are too severe to reverse with better diabetes control alone, keeping your blood glucose levels in line can help to prevent further damage. Another tip: Quit smoking. It’s linked to sexual problems, and it’s all-around bad news for the rest of your body.
There are several approaches that both men and women benefit from, including seeing a doctor who specializes in sexual medicine and talking with a mental health professional. The latter is an important step because relationship problems, body issues, stress, and a host of other emotional baggage can affect all aspects of your sex life. You may be too self-conscious to get in the mood or get aroused, or maybe you’re too stressed to have an orgasm.
A counselor can also help you and your partner work out any strain your sexual dysfunction may have caused. “It creates such emotional tension in a relationship that it permeates the entire relationship, not just in the bedroom,” Roszler says. So talk it out and find a way to work around your sexual problems.
Finally, consider making lifestyle changes. Managing your diabetes well, including eating healthfully, exercising regularly, and reducing stress, will benefit your entire body, not just your nether regions. “I think it’s very likely that a good sex life leads to better health,” says Lindau. “And better health leads to good sex.”
Source: diabetesforecast.org